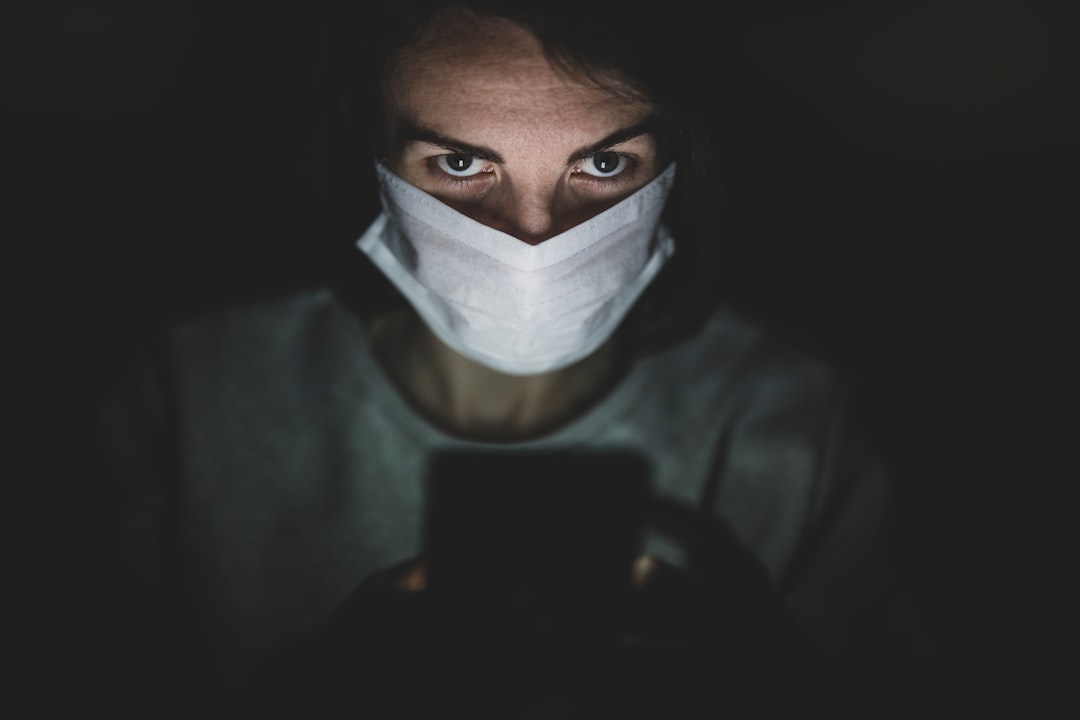
Nurse burnout has emerged as a critical issue within the healthcare sector, characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment. This phenomenon is often the result of prolonged exposure to high-stress environments, where nurses are required to manage heavy workloads, complex patient needs, and emotional demands. The relentless pace of healthcare, particularly in acute settings, can lead to a state where nurses feel overwhelmed and unable to cope effectively.
As they navigate the challenges of their roles, the risk of burnout increases, ultimately affecting their well-being and the quality of care they provide. The implications of nurse burnout extend beyond individual health; they can ripple through entire healthcare systems. When nurses experience burnout, their ability to deliver compassionate and effective care diminishes.
This not only affects patient outcomes but can also lead to increased turnover rates among nursing staff, further exacerbating staffing shortages and creating a vicious cycle. Understanding the root causes of nurse burnout is essential for developing effective strategies to mitigate its effects and foster a healthier work environment for nursing professionals.
Key Takeaways
- Nurse burnout is a serious issue that can lead to decreased job satisfaction and increased turnover.
- Nurse burnout can negatively impact patient care, leading to medical errors and decreased quality of care.
- Strategies for addressing nurse burnout include promoting work-life balance and providing support and resources for nurses.
- Hospital queues can have a significant impact on patient satisfaction and overall hospital efficiency.
- Factors contributing to hospital queues include inefficient processes and lack of communication between departments.
Recognizing the Impact of Nurse Burnout on Patient Care
The impact of nurse burnout on patient care is profound and multifaceted. Research has consistently shown that when nurses are burned out, the quality of care they provide suffers significantly. This can manifest in various ways, including increased medication errors, longer response times to patient needs, and a general decline in the attentiveness that patients receive.
Burned-out nurses may struggle to maintain the empathy and compassion that are crucial for effective patient interactions, leading to a less supportive environment for those in their care. Moreover, the consequences of nurse burnout can extend to patient safety. Studies have indicated that higher levels of nurse burnout correlate with increased rates of adverse events in healthcare settings.
Patients may experience longer hospital stays, higher readmission rates, and even worse health outcomes as a result of inadequate nursing care. Recognizing the link between nurse burnout and patient care is vital for healthcare administrators and policymakers who aim to improve both nurse well-being and patient safety.
Strategies for Addressing Nurse Burnout

Addressing nurse burnout requires a multifaceted approach that encompasses organizational change, individual support, and systemic improvements. One effective strategy is to implement wellness programs that focus on mental health resources, stress management techniques, and resilience training. These programs can provide nurses with tools to cope with the demands of their roles while fostering a culture of support within healthcare organizations.
By prioritizing mental health, institutions can help mitigate the effects of burnout and promote a healthier work environment. Another critical strategy involves reassessing staffing levels and workload distribution. Ensuring that nurses have manageable patient loads is essential for reducing stress and preventing burnout.
Organizations can explore innovative staffing models that allow for greater flexibility and support during peak times. Additionally, fostering open communication channels where nurses can voice their concerns about workload and stressors can empower them to advocate for necessary changes within their work environments.
Importance of Addressing Hospital Queues
| Metrics | Data |
|---|---|
| Average wait time | 45 minutes |
| Number of patients waiting | 30 |
| Percentage of patients leaving without being seen | 15% |
| Impact on patient satisfaction | Decreased |
| Effect on hospital reputation | Negative |
Hospital queues represent a significant challenge within healthcare systems, often leading to increased patient dissatisfaction and compromised care quality. Long wait times can create frustration for patients seeking timely medical attention, which can exacerbate their health conditions and lead to negative experiences within the healthcare system. Addressing hospital queues is not merely an operational concern; it is a matter of patient-centered care that directly impacts health outcomes.
Furthermore, long queues can contribute to nurse burnout as well. When nurses are faced with an influx of patients waiting for care, they may feel pressured to rush through assessments and treatments, leading to increased stress levels and potential errors in care delivery. By addressing hospital queues effectively, healthcare organizations can alleviate some of the burdens placed on nursing staff while simultaneously enhancing the overall patient experience.
Impact of Hospital Queues on Patient Satisfaction
The relationship between hospital queues and patient satisfaction is well-documented in healthcare literature. Patients who experience long wait times often report lower satisfaction levels with their overall care experience.
In an era where patient-centered care is paramount, understanding how queues affect satisfaction is crucial for healthcare leaders aiming to improve service delivery. Moreover, patient satisfaction is increasingly linked to health outcomes. When patients feel valued and receive timely care, they are more likely to adhere to treatment plans and engage in their health management actively.
Conversely, long wait times can lead to disengagement and frustration, potentially resulting in poorer health outcomes over time. Therefore, addressing hospital queues not only enhances patient satisfaction but also contributes to better overall health management.
Identifying Factors Contributing to Hospital Queues

Understanding the factors contributing to hospital queues is essential for developing effective solutions. Several elements can lead to increased wait times, including inadequate staffing levels, inefficient triage processes, and high patient volumes during peak hours. Additionally, systemic issues such as lack of access to primary care services can funnel more patients into emergency departments, exacerbating queue problems.
Another contributing factor is the variability in patient needs. Some patients may require more complex care than others, leading to longer treatment times that can slow down the overall flow within the hospital. Identifying these factors allows healthcare administrators to target specific areas for improvement, ultimately leading to more efficient operations and reduced wait times for patients.
Implementing Solutions to Reduce Hospital Queues
To effectively reduce hospital queues, healthcare organizations must adopt a proactive approach that includes both short-term fixes and long-term strategies. One immediate solution could involve optimizing triage processes to ensure that patients are assessed quickly and directed to appropriate care settings based on their needs. Implementing fast-track systems for less critical cases can also help alleviate congestion in emergency departments.
In the long term, investing in community-based care initiatives can significantly reduce the burden on hospitals by providing patients with alternative options for non-emergency medical needs. By enhancing access to primary care services and preventive measures, hospitals can decrease the influx of patients seeking urgent care, thereby reducing queues and improving overall patient flow.
The Role of Technology in Addressing Hospital Queues
Technology plays a pivotal role in addressing hospital queues by streamlining processes and enhancing communication among healthcare providers.
Additionally, telemedicine solutions enable patients to receive care remotely for non-urgent issues, reducing the need for in-person visits that contribute to hospital congestion.
Moreover, implementing queue management systems can provide real-time data on patient flow within hospitals. These systems allow administrators to monitor wait times actively and make informed decisions about resource allocation based on current demand. By leveraging technology effectively, healthcare organizations can create a more responsive system that minimizes wait times while maintaining high-quality care standards.
Collaborating with Interdisciplinary Teams to Address Hospital Queues
Collaboration among interdisciplinary teams is essential for tackling the complex issue of hospital queues effectively. By bringing together professionals from various specialties—such as nursing, medicine, administration, and social work—healthcare organizations can develop comprehensive strategies that address the root causes of congestion. This collaborative approach fosters a shared understanding of challenges and encourages innovative solutions tailored to specific needs.
Interdisciplinary teams can also enhance communication across departments, ensuring that all staff members are aligned in their efforts to reduce wait times. Regular meetings and collaborative problem-solving sessions can help identify bottlenecks in patient flow and develop targeted interventions that improve efficiency while maintaining high standards of care.
Improving Communication to Reduce Hospital Queues
Effective communication is a cornerstone of successful queue management within hospitals. Clear communication among staff members regarding patient needs and flow can significantly reduce delays in care delivery. Implementing standardized protocols for handoffs between shifts or departments ensures that critical information is conveyed accurately and promptly.
Additionally, enhancing communication with patients themselves is vital for managing expectations around wait times. Providing patients with real-time updates about their status in the queue or estimated wait times can alleviate anxiety and improve their overall experience within the hospital setting. By prioritizing communication at all levels, healthcare organizations can create a more efficient system that benefits both patients and providers.
Monitoring and Evaluating the Effectiveness of Interventions for Nurse Burnout and Hospital Queues
Monitoring and evaluating the effectiveness of interventions aimed at reducing nurse burnout and hospital queues is crucial for ensuring continuous improvement within healthcare systems. Establishing key performance indicators (KPIs) related to nurse well-being—such as turnover rates, job satisfaction scores, and burnout assessments—can provide valuable insights into the impact of implemented strategies. Similarly, tracking metrics related to hospital queues—such as average wait times, patient throughput rates, and satisfaction scores—can help organizations assess the effectiveness of their queue management initiatives.
Regularly reviewing these metrics allows healthcare leaders to identify areas for further improvement and make data-driven decisions that enhance both nurse well-being and patient care quality over time. In conclusion, addressing nurse burnout and hospital queues requires a comprehensive approach that considers both individual well-being and systemic efficiency. By understanding the complexities surrounding these issues and implementing targeted strategies, healthcare organizations can create a healthier work environment for nurses while simultaneously improving patient experiences within the system.
Through collaboration, technology integration, effective communication, and ongoing evaluation efforts, it is possible to foster a more resilient healthcare system that prioritizes both provider satisfaction and patient outcomes.
Nurse burnout has become a pressing issue in healthcare, particularly as it contributes to longer hospital queues and decreased patient care quality. A related article that delves into the complexities of this problem can be found at this link. It explores the factors leading to nurse burnout and its impact on hospital efficiency, highlighting the urgent need for systemic changes to support healthcare professionals.
WATCH THIS! Why Australia’s Middle Class Is Disappearing
FAQs
What is nurse burnout?
Nurse burnout is a state of physical, emotional, and mental exhaustion caused by prolonged and excessive stress. It can lead to feelings of cynicism, detachment from work, and a sense of ineffectiveness.
What are the causes of nurse burnout?
Nurse burnout can be caused by factors such as heavy workloads, long hours, lack of support from management, inadequate staffing, and exposure to traumatic events.
What are the consequences of nurse burnout?
Consequences of nurse burnout can include decreased job satisfaction, increased risk of medical errors, higher turnover rates, and negative impacts on patient care and safety.
How can nurse burnout be addressed?
Nurse burnout can be addressed through measures such as improving staffing levels, providing support and resources for nurses, implementing wellness programs, and promoting a positive work environment.
What are hospital queues?
Hospital queues refer to the waiting lines that form in hospitals, where patients wait for various services such as consultations, tests, and treatments.
What are the impacts of hospital queues?
Hospital queues can lead to increased patient dissatisfaction, longer wait times for care, and potential delays in receiving necessary medical attention.
How can hospital queues be managed?
Hospital queues can be managed through strategies such as improving scheduling and appointment systems, optimizing workflow processes, and allocating resources effectively to reduce wait times.